Eye Disease Diagnosis
Frequently, individuals are not aware of how prevalent eye diseases are. Millions of people are exposed to potentially serious eye conditions that may eventually lead to vision loss.
Some eye conditions can be treated if caught early. Prevention is imperative to preserving healthy eyes and clearer vision.
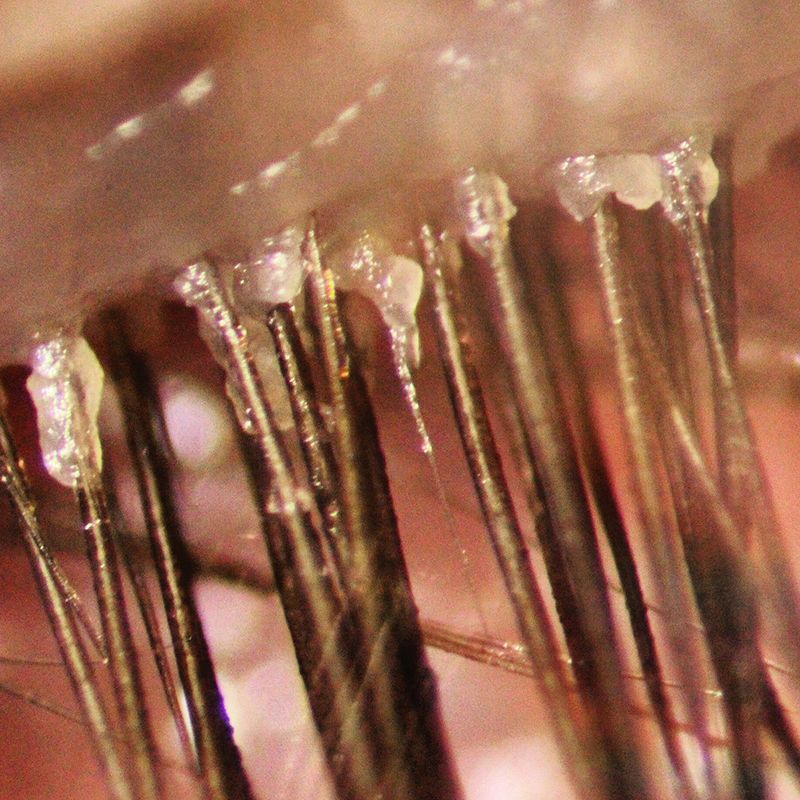
Blepharitis is inflammation of the eyelids. It is a very common disorder in which the lid becomes red, swollen, itchy, crusty and dandruff-like scales form on the eyelashes. It may be associated with a low-grade bacterial infection or a skin condition known as seborrheic dermatitis.
Blepharitis occurs in two forms: anterior blepharitis and posterior blepharitis.
Blepharitis Treatments
Blepharitis Causes
Bacterial infection: Bacteria, such as Staphylococcus aureus, can infect the eyelid margins, leading to inflammation and irritation.
Demodex mites: Overgrowth of Demodex mites on the eyelids can cause irritation and inflammation, resulting in a type of blepharitis known as Demodex blepharitis.
Meibomian gland dysfunction (MGD): Dysfunction of the meibomian glands, which produce the oily layer of the tear film, can lead to blockage of the glands and inflammation of the eyelids.
Allergic reactions: Allergens, such as pollen, pet dander, or cosmetics, can trigger allergic reactions on the eyelids, causing blepharitis symptoms.
Seborrheic dermatitis: A common skin condition characterized by red, scaly patches, seborrheic dermatitis can also affect the eyelids and lead to blepharitis.
Poor eyelid hygiene: Inadequate eyelid hygiene, such as not removing makeup or debris from the eyelids, can contribute to the development of blepharitis.
Contact lens wear: Improper hygiene practices or wearing contact lenses for extended periods can increase the risk of developing blepharitis.
It's important to identify the underlying cause of blepharitis in order to determine the most appropriate treatment approach and best course of action based on individual circumstances.
Blepharitis treatments
Lid Scrubs: Eyelid scrubs performed by a healthcare professional can help remove debris, crusts, and excess oil from the eyelids, which can reduce the mite population.
BlephEx: This is a procedure performed by an eye care professional using a specialized device to mechanically remove debris and exfoliate the eyelids, helping to eliminate Demodex mites and improve symptoms.
Thermal Pulsation Therapy: This treatment involves applying controlled heat to the eyelids to liquefy and remove hardened oils and debris, which can harbor Demodex mites.
Intense Pulsed Light (IPL) Therapy: IPL therapy utilizes pulses of light to target and destroy Demodex mites and their eggs, while also reducing inflammation and improving overall eyelid health.
Prescription Medications: In some cases, our doctors may prescribe topical or oral medications, such as tea tree oil-based cleansers, antibiotics, or anti-inflammatory agents, to help to control the blepharitis and alleviate symptoms.
It's important to consult with an eye care professional to determine the most appropriate in-office treatment for Demodex blepharitis based on the severity of the condition and individual needs. Additionally, maintaining good eyelid hygiene practices at home, such as regular eyelid cleaning and using prescribed medications as directed, can help prevent recurrence of Demodex infestation.
Posterior blepharitis affects the inner surface of the eyelid that comes in contact with the eye. It is usually caused by problems with the oil (meibomian) glands in the lid margin. Posterior blepharitis is more common than the anterior variety and often affects people who have rosacea.
Meibomian Gland Dysfunction
There is a blockage of the small glands, which are located in the inner surface of the eyelid. These sebaceous glands are responsible to release lipids (oil) into the tear film. Once the glands become inflamed, they become obstructed and unable to release the oil, hence eyes become dry.
Blepharitis Signs and Symptoms
Regardless of which type of blepharitis you have, you will probably experience eye irritation, burning, tearing, foreign body sensation, crusty debris (in the lashes, in the corner of the eyes or on the lids), dryness and red eyelid margins.
It is imperative to consult an eye doctor and obtain treatment. If your blepharitis is bacterial, possible long-term effects are thickened lid margins, dilated and visible capillaries, misdirected eyelashes, loss of eyelashes and a loss of the normal position of the eyelid margin against the eye. Blepharitis can also lead to styes and infection, along with erosions of the cornea.

Commonly known as pink eye. This occurs when the thin transparent layer of tissue that covers the inner surface of the eyelid and the white part of the eye, becomes irritated and inflamed. It may be caused by different agents: allergies, viruses or bacteria.
Allergic Conjunctivitis
It generally affects both eyes. May experience teary, red, itchy and swollen eyelids. You experience allergic conjunctivitis when your body tries to defend itself against a perceived threat. For instance, pollen from trees and grass as well as animal dander. There are various treatment methods.
– For mild allergic reactions, lubrication with artificial tears and cool compresses.
– In more severe cases, Optometrist will prescribe anti-allergic drops to ease the symptoms away.
Bacterial Conjunctivitis
May experience mucous greenish discharge, burning, eyelids stuck together upon awakening, discomfort, light sensitivity but there is no pain. Bacterial conjunctivitis is caused by bacteria that infect the eye through various sources of contamination. It is contagious, therefore it is critical to maintaining proper hygiene, so as to not contaminate or expose others. This condition is usually self-limited, it usually lasts for 1 or 2 weeks, however, it can also be treated with topical antibiotics to reduce the length of the symptoms and reduce the risk of contaminating others.
Viral Conjunctivitis
May experience irritation, tearing and sensitivity to light. The infection starts in one eye and rapidly spreads to the other eye. Different viruses lead to Viral conjunctivitis. It is highly contagious, as airborne viruses can be spread through sneezing and coughing. In addition, Viral conjunctivitis can also come from common viral upper respiratory infections such as measles, the flu or the common cold. Viral conjunctivitis is self-limited; it will dissipate on its own after a short period of time. No eye drops or ointments are effective against the common viruses that cause viral conjunctivitis.
For a reliable and accurate assessment of your symptoms, book an appointment with us.
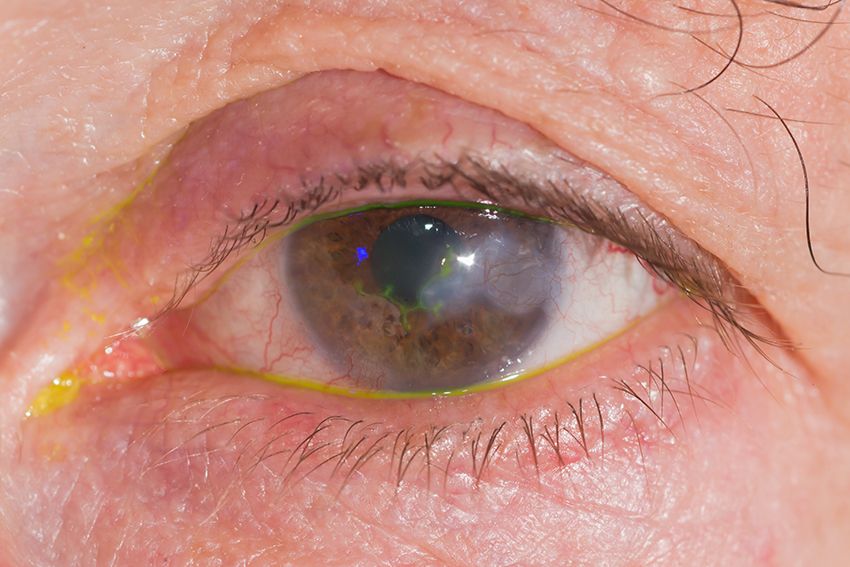
Keratitis is an inflammation of the cornea (the transparent membrane covering the iris and pupil). The common symptoms are a red eye, foreign body sensation, pain, sensitivity to light, and watery eyes.
Bacterial Keratitis or Corneal Ulcer
The cornea is infected by bacteria. A common type of bacteria that commonly causes bacterial keratitis is Pseudomonas Aeruginosa. It is a vision-threatening condition; bacteria can perforate the cornea in 48 hours. Bacterial keratitis is mostly seen in contact lens wearers.
- Patients who tend to sleep with their contact lenses.
- Patients who do not replace contact lenses at a specific time.
- Patients who do not disinfect contact lenses well.
- Patients store or rinse contact lenses in water.
- Patients who do not clean contact lens cases.
Patients develop severe pain, eye redness, blurred vision, sensitivity to light, excessive tearing, and eye discharge. Generally, treatment starts empirically with broad-spectrum antibiotic eye drops. If the corneal ulcer is not in the center of the cornea, the consequences can be minimal, but if it is in the center, it may leave a permanent scar, resulting in permanent vision loss.
If you are a contact lens wearer and develop any of the symptoms above, do not wait, call your eye doctor so you can start a course of medical therapy.

It is a condition in which the cornea thins and bulges into a cone shape causing distorted vision. According to the Global Keratoconus Foundation, the condition occurs in 50 to 230 patients per 100,000 and in men and women of all races.
The cornea is the clear tissue on the outermost surface of the eye covering the iris (color tissue) and pupil. The main function of the cornea is to refract light entering the eye.
A normal cornea will have a smooth shape. A cornea with an ectasia will have an irregular shape or bulge. This irregular corneal shape does not refract light correctly and will create irregular and distorted vision. Ectasias can be caused by corneal problems such as keratoconus, or may result after a surgery such as LASIK, or after injury to the eye.
Common Symptoms
Symptoms first appear during puberty or late teens
- Glare sensitivity and increase sensitivity to light
- Difficulty reading regular print
- Difficulty with work or activities requiring near vision
- Complaint of pain
Blurry Vision
Treatment
Treatment for keratoconus depends on the severity of the condition and how quickly the condition is progressing. There are surgical and non surgical treatment methods. Mild to moderate keratoconus can be treated with eyeglasses or contact lenses. In more advance cases, surgery might be necessary.
Avoid rubbing the eyes
Rubbing the eyes damages the thin layers of your cornea, make your symptoms worse and possibly increase your risk of Keratoconus.
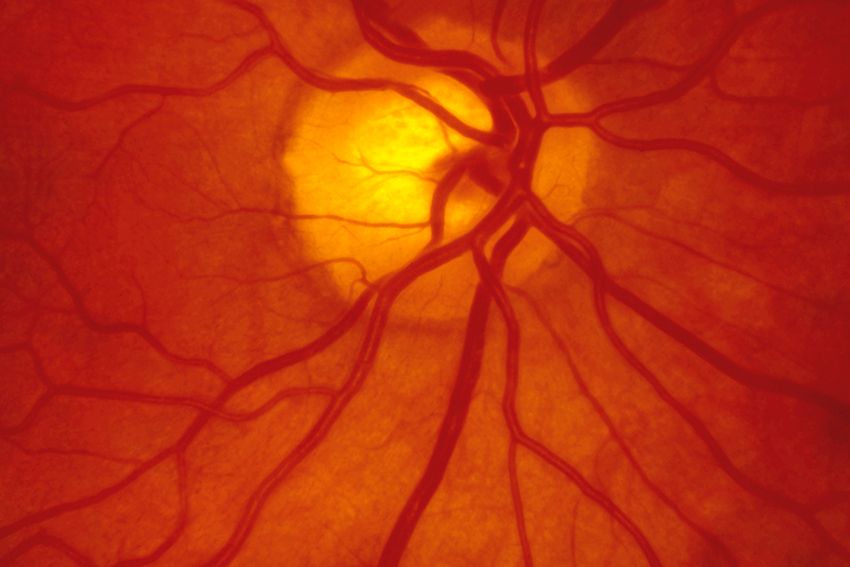
Glaucoma refers to a category of eye disorders that results in damage to the optic nerve. There is no cure for glaucoma, hence once vision is lost, it can’t be recovered.
Glaucoma is currently the second leading cause of blindness in the United States, It is estimated that over 3 million Americans have glaucoma, however, only half of the estimated population are aware that they have it.
Glaucoma typically affects your peripheral vision first. This is why it is such an insidious disease. As a result, you can lose a great deal of your vision from glaucoma, even before you are well aware anything is happening. If uncontrolled or left untreated, glaucoma can eventually lead to blindness.
Risk Factors
- High eye pressure
- Family history of glaucoma
- Ethnicity plays a critical role in certain types of glaucomas
- Eye anatomy
- Cardiovascular diseases
- Diabetes
- Eye injury
Symptoms of Glaucoma
Glaucoma is often referred to as the “silent thief of sight,” most types of glaucoma typically cause no pain and have no symptoms. For this reason, glaucoma often progresses undetected until the optic nerve already has been irreversibly damaged; with varying degrees of permanent vision loss.
There are other forms of the disease (acute angle-closure glaucoma), where symptoms of blurry vision, halos around lights, intense eye pain, nausea, and vomiting occur suddenly. If you have any of these symptoms, make sure you see an eye care practitioner immediately or visit the emergency room, so steps can be taken to prevent permanent vision loss.
What Causes Glaucoma?
There is not an exact cause of glaucoma, however, It is generally associated with failure of the eye to maintain an appropriate balance between the amount of fluid produced inside the eye and the amount that it’s drained out. The drainage system is not able to evacuate fluid out of the eye, therefore leading to a gradual build-up of fluid pressure (IOP) inside the eye.
Early Detection Is Key
Regardless of the treatment, early diagnosis is the optimal way to prevent vision loss from glaucoma. See your eye care practitioner routinely for a complete eye examination, including a check of your IOP.
Allow Dussan Eye Care to manage your risk of vision loss. Make an appointment for a comprehensive eye exam.
A cataract is any cloudiness of the natural lens of the eye, which is normally crystal clear. Some cataracts are small and do not interfere with vision. People with small cataracts may experience no visual problems. Nevertheless, large cataracts can cause:
- Blurry vision
- Ghost images
- Double vision in one or both eyes
- Faded colors and halos of lights.
- Glare sensitivity for headlights and sun
Why do get cataracts?
Most cataracts will develop with age. However, other factors can contribute to cataract development:
- Diabetes
- Poor diet
- Smoking
- Alcohol
- Exposure to harmful un ligh
Type of Cataracts
Nuclear Sclerotic Cataracts
This is the most common type of age-related lens changes (senile), caused primarily by the hardening and yellowing of the lens over a long period of time. This starts in the center (nucleus) of the crystalline lens.
Cortical Cataracts
Usually age-related. It starts in the periphery of the lens and works its way to the center in a spoke-like fashion.
Posterior Subcapsular Cataracts (PSC)
A usually induced related cataract starts towards the back of the lens. It is often the result of treatment steroid medication or other causes such as smoking and not wearing UV protection sunglasses. They significantly affect vision and provoke halos around the lights. PSC requires more aggressive approaches and may lead to surgery at a much faster pace than other types of cataracts.
Secondary Cataracts
It happens after a patient undergoes cataract surgery. The implant is placed in the natural sac. A cloudy layer of scar tissue forms behind your lens implant. It is called Posterior capsular opacity (PCO). Yag laser Treatment is necessary to clean up the sat tissue, covering the implant or intraocular- lens.
Traumatic Cataracts
This occurs after a blunt or penetrating trauma to the eye or head. People can develop a traumatic cataract at any age and they tend to develop fast and stable.
How to Prevent Cataracts
There is no scientific evidence that displays ways in which cataracts may be prevented, however, there are certain steps we can implement to delay their occurrence.
- Avoiding excessive sunlight exposure, limiting alcohol consumption, and quitting smoking.
- Eating plenty of fresh veggies and fruits.
- Vitamin A, C, E, Z
- Fish and omega-3
Cataract Treatment
The only way to treat cataracts is with surgery.

Macular degeneration is a condition where the central area of the retina (macula) breaks down, leading to gradual vision loss. This region is responsible for the visual of colors and fine details. Advance macular degeneration (AMD) is the leading cause of blindness in people age 50 and over.
Types of macular degeneration
Dry macular degeneration
It is the most common type of macular degeneration; affecting 90 % of individuals with AMD. At the beginning stages of the disease, the macula displays a change in its color (pigment), and also waste deposits (drusen) can be seen on the surface of the retina. During this stage, there may be some vision loss, but they’re still may not be noticeable symptoms. The patient may very well have a 20/20 vision.
Early detection and prevention is a key factor. For all patients with risk of developing macular degeneration or are in initial stages of the disease, lifestyle changes and special nutrition are recommended. Eye vitamins or supplements have not shown to be beneficial. They do not seem to cause harm, however, they have no benefits in delaying the progression of the disease.
Wet macular degeneration
Affects from 10-15 % of individuals with macular degeneration.
Unfortunately, some patients will progress to a more serious stage known as, wet age-related macular degeneration, where abnormal blood vessels under the retina begin to grow toward the macula. Due to the fact that these new blood vessels are abnormal, they tend to break, bleed, and leak fluid, These vessels can leak fluid and blood, which may lead to swelling and damaging the macula. This can result in a rapid and severe loss of central vision.
These patients are referred to a retinal specialist for assessment and usually will be injected with Anti-VEGF medicine such as Avastin. This drug can either remove or control the blood vessels growing beneath the eye. Science has made tremendous progress in the last 10-15 years. Drugs available, currently can save a patient’s vision and slow down the progression of the disease.
During your exam at our office, we advised our patients to suspend smoking, we recommend blue light protection; additionally, recommend our patients to increase the consumption of dark green leafy vegetables, which contain carotenoids (lutein and zeaxanthin) that may serve to protect the macula from damaging blue light.
Again, a routine eye exam is an optimal measure to ensure you don’t have early macular degeneration.
https://www.allaboutvision.com/conditions/amd-prevention.htm
What is Diabetic Retinopathy?
Diabetic retinopathy is an eye condition that occurs in people who have either Type 1 or Type 2 diabetes. Consistent high blood sugar from diabetes compromises the integrity of the tiny vessel walls in the retina, altering their structure and function. These fragile vessels may thicken, bleed, develop clots, develop balloon-like causing retinal tissue to swell and damage the cells in the retina.
In the early stages of diabetic retinopathy, they are usually no warning signs. The disease often progresses unnoticed until it affects vision. Bleeding from abnormal retinal blood vessels can cause the appearance of “floating” spots. These spots sometimes clear on their own. So the vision is not affected.
In most advanced stages, new abnormal blood vessels proliferate (increase in number) on the surface of the retina; fluid accumulates in the central part of the eyes resulting in changes or loss of central vision. Fluid also can lead to scarring and separation of the retina from the other layers of the eye (retinal detachment) increasing the risk of permanent vision loss.
Eye Exam
Diabetic eye disease can be effectively detected through a comprehensive diabetic eye exam which includes different testing procedures. Our Dr in Long Island City would take a careful medical history. We need to know the nature of your diabetes (Type 1 or type 2), the duration of the disease, your fasting blood glucose level for that day as well as your hemoglobin A1C, which indicates your average blood glucose for the 3 months prior.
An exam is then performed with a careful dilated eye examination looking for any signs of diabetic retinopathy. We will send a report of findings to your primary care physician. If no signs of diabetic retinopathy are detected, the diabetic eye exam should be repeated yearly.
If the level of diabetic retinopathy warrants it, you will be referred to a retinal specialist for treatment.
Treatment for Diabetic Retinopathy
Treatment is based on the severity of the disease. Unfortunately, there are no non-invasive treatments.
Early Diabetic Retinopathy
Early or moderate non-proliferative diabetic retinopathy may not need treatment right away and an accurate blood sugar control can slow the progression of the disease.
Advance diabetic Retinopathy
In more advanced cases Proliferative diabetic Retinopathy or swollen the central area of the retina (macular edema) may require laser treatment or surgery.
Even after treatment for diabetic Retinopathy, your Doctor may require to follow up appointments to make sure the treatment was effective. Our doctor works with the most experienced Ophthalmologist (Retinal Specialist) to refer patients out when it is necessary and ensure you receive the outmost care in the area. Call us today for more information regarding our services.
To learn about about Diabetic Retinopathy:
https://nei.nih.gov/health/diabetic/retinopathy

Retinal detachment
Retinal detachment is a painless sight-threatening eye problem that is associated with a number of symptoms and warning signs that occur before the actual detachment happens.
What is the retina?
The Retina is a thin layer of tissue that lines the back wall of your eye, it is responsible for absorbing light and converting it into an electrical signal that is sent to the brain via the optic nerve, allowing us to see.
What is a retinal detachment?
A retinal detachment occurs when the retinal layers separate. Any portion of the retina that is detached can not send visual signals to the brain.
Types of retinal detachment
There are three main types of retinal detachments
- Rhegmatogenous detachment
The most common type. Happens when there is a hole or tear in the retina. This hole allows fluid to slip through the opening and get behind the retina. Fluid separates the retina form a layer that provides nourishment and oxygen to the retina, causing the retina to separate.
- Traditional retinal detachment
It happens when scar tissue on the retina’s surface contracts and causes your retina to pull away from the back of your eye.
- Exudative retinal detachments
There are not breaks or holes in your retina. Certain Retinal diseases can cause a detachment.
- An inflammatory disorder causing fluid accumulation behind your retina
- Cancer behind the retina
- Coat’s disease, which causes abnormal development in the blood vessels cause leaking of proteins behind the retina.
What are the risk for a retinal detachment
- Patients who have poorly control of diabetes
- People Lattice degeneration
- People that are extreme near sighted
- People with family history of retinal tears or retinal detachment
- People previous cataract, glaucoma surgery or any other surgery
- Severe eye injury or trauma
Symptoms of retinal detachment
- Sudden and dramatic increase in floaters
- Sudden decrease in vision
- Flashes of lights
- A gray curtain moving across your field of vision
- Straight lines appearing curve
How to prevent retinal detachment?
There is no way to prevent a Retinal detachment. However, you can avoid a retinal detachment that results from an injury by wearing protective eyewear.
If you experience any symptom of retinal detachment, go immediately to your eye doctor.
Comprehensive dilated eye exams regularly can help to detect small tears or retinal detachment early.
Treatment
The sooner a detached retina is treated, the better the chance of a good outcome. If a retinal tear is detected early, Retinal specialists can often weld down. In the case of retinal detachment surgery is almost always necessary.
The goal of treatment is to reattach the retina to the back wall of the eye and seal the tears or holes that caused the detachment. There are several approaches to repair a retinal detachment. Base on the characteristics of the detachment a Retinal specialist can determine which approach is more suitable.










